
Dr. Mark Gold's Research You Can Use
This series of four articles explores more evidence-based, accessible and comprehensive treatment and mitigation options to treat the OUD Epidemic, prioritizing, and above all, saving lives. This second article of the series talks in greater depth about the dire necessity of improving existing treatments. Clearly, we need better and more effective treatment, but in the meantime, we need to make what we have, work better.
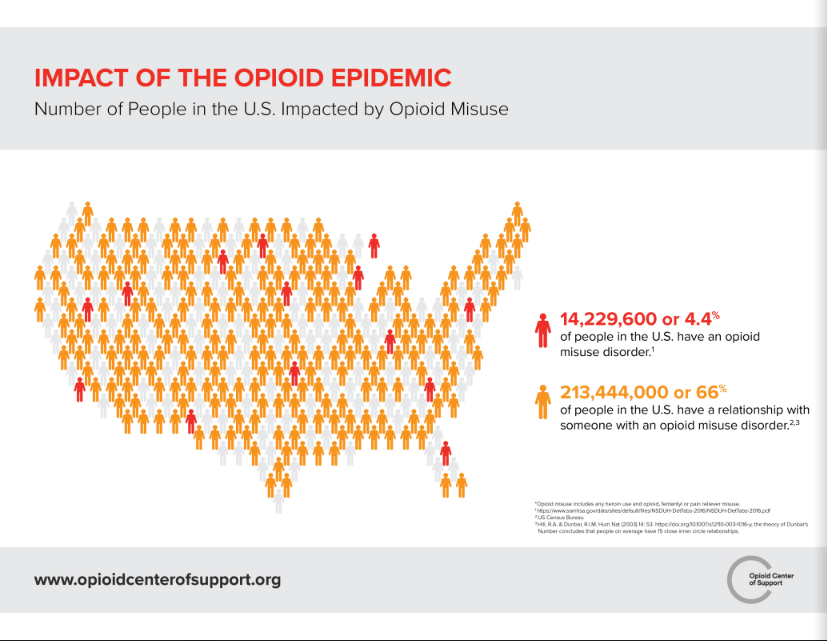
After the vastly debilitating HIV/AIDS pandemic that the United States survived through, the current opioid misuse and overdose emergency is the next catastrophic crisis of epidemic proportions. Current national trends indicate that more people die of overdoses annually, the majority of which involve opioid drugs, compared to the fatalities in the entirety of the Vietnam War, the Korean War, or any armed conflict since the end of World War II.
Treatment for opioid addiction or overdoses is more than just detoxification. Opioid addiction is complex. In the face of recent findings, it is more and more clear that addiction is a chronic, lifelong, and relapsing disease. It shortens life, diminishes the quality of life, and even when treatment is successful, the addict and family wonder whether things will ever return to the way they were before the substance of abuse took over.
Addiction requires an all-encompassing approach to counter the drug-addict bond. While the focus remains largely upon opioids, there are many other factors of a patient’s life and co-occurring disorders that need to be prioritized in order to make treatments more effective.
In addition to medication-assisted treatment (MAT), office-based opioid treatments and ambulatory detoxification, timely identification and treatment of co-existing trauma, sexually transmitted diseases, infections, cardiovascular and other common psychological co-occurring disorders have to take its due position in recovery.
Addiction is a chronic brain disease and importance of MATs
 It is important to understand that addiction is a chronic brain disease and that people can become addicted by taking medication exactly as prescribed.
It is important to understand that addiction is a chronic brain disease and that people can become addicted by taking medication exactly as prescribed.
Being addicted to opioids means a person forms a relationship with a drug which dwarfs other relationships, work, community, and health.
The addict naturally loses control of their drug use and then their lives. In contrast, someone can be physically dependent on opioids without becoming addicted.
Nevertheless, addiction is often not treated or managed the same as other chronic diseases. Understanding that addiction impairs the brain helps identify an important array of effective interventions and preventions.
The science of addiction has revealed that an addicted person’s impaired ability to stop abusing drugs is related to deficits in the function of the prefrontal cortex part of the brain involved in executive function, self-monitoring, and prioritization.
Hence, many religious people rely on the patient’s saying no to drugs as the protective factor. But, for most, just saying no is not enough. Once addicted, the patient needs to slowly and purposefully re-learn and develop alternative sources of joy and reward, which can only be accomplished through a holistic treatment approach.
Just as addiction cannot be classified as a moral failing, it cannot be over-simplified as “all biology.” The idea is to mitigate the self-loathing and guilt among patients in order to help them embark on recovery toward a better life.
This is achievable only when each patient is treated with an individualized recovery plan, focusing on all biological, mental, social and emotional needs. Treatments cannot solely rely on MATs neither can they ignore the importance of medications altogether.
As discussed in much detail in the first article of this series, an OUD or opioid addiction is a disease, and it needs the help of medications at times or for extended periods of time because of the nature of this deadly disease.
Physician’s Health Programs- the gold standard?
One of the prime public health achievements of the past half-century has been changes in the way physicians treated fellow physicians with alcohol and other drug problems. States created a novel system of specialty treatment programs for their colleagues with substance abuse problems. Replicable models upon which the modern treatment system was built, all surfaced between 1944 and 1970.
 The movement to treat a SUD instead of punishing addiction problems peaked in the early 1970s, as the infrastructure of modern addiction treatment emerged, based predominantly on two events: return of a large number of addicted Vietnam era veterans and secondly, policy changes within insurance companies that provided reimbursement for alcoholism treatment under private health insurance.
The movement to treat a SUD instead of punishing addiction problems peaked in the early 1970s, as the infrastructure of modern addiction treatment emerged, based predominantly on two events: return of a large number of addicted Vietnam era veterans and secondly, policy changes within insurance companies that provided reimbursement for alcoholism treatment under private health insurance.
These changes marked a shift in the nation’s long-standing strategy of handing over addicts to law enforcement toward a more balanced strategy that included foremost prevention, timely intervention, and treatment.
Initiated in 2005, Bob Dupont, Tom McLellan and I with researchers from the Institute for Behavior and Health and the Treatment Research Institute collaborated with the Federation of State Physician Health Programs to study the PHP supervised treatment of addicted physicians.
904 physicians were successively admitted to 16 state Physicians Health Programs (PHPs) and studied for five years or longer to categorize the outcomes of care and further examine the elements of these programs that could improve the care of other addicted populations. The study firstly characterized the PHPs and their system of care management and then continued to describe the outcomes as recorded.
The programs were abstinence-based, requiring physicians to abstain from any use of alcohol or other drugs of abuse, assessed by frequent random tests over the course of five years. Tests rapidly identified any return to substance use, leading to swift and significant consequences. Exceptionally, 78 percent of participants had no positive test for substance use over the 5-year period of intensive monitoring.

At post-treatment follow-up, 72 percent of the physicians continued to practice medicine.
The unique PHP care management maintained close ties to the 12-step programs of Alcoholics Anonymous and Narcotics Anonymous, alongside utilizing residential and outpatient treatment programs that were selected based on merit.
The results were not influenced by the physician's drug of choice.
Instead, physicians with alcohol use disorders displayed similar outcomes to those dependent on opioids, crack cocaine and benzodiazepine. Physicians using these drugs intravenously performed as well as other participants.
There is no such solution as a “quick” treatment
Physician addicts are frequently tested for use, evaluated and treated for five years and sometimes more. There were significantly positive and negative consequences to noncompliance with the program.
Such use of “socially sanctioned coercion mechanisms” have proven to improve treatment outcomes in the long term significantly.
Unfortunately, many modern addiction treatments are virtually short-term. It is difficult to comprehend how a disease developed over years of abuse and neglect, can be treated by just detox of 10 days or even less.
Such short-term treatments falsely give patients and families the idea that addiction treatment is some sort of quick fix. In reality, such short-sighted treatments may only be delaying further misuse and even overdose. The disease of addiction is an acquired, chronic, lifelong disease.
It is clear from simply following celebrity relapses that the risk of relapse remains even after years of stable recovery. Recovery or “remission” of the symptoms of the disease of addiction, is the ultimate goal of treatment. Care needs to continue in terms of frequent testing, therapy, counseling, and self-care.
Treating comorbidities
Beyond overdose deaths, OUD is almost always accompanied with severe medical and psychiatric consequences that need treatment. Experts in neurology, infectious diseases, internal medicine, cardiology, oncology, psychiatry, sociology, dentistry, public health, and criminal justice have written extensively about the co-occurring diseases associated with
intravenous heroin uses and dependence.
Cardiovascular, neurovascular and immunological systems of opioid users are compromised as a direct consequence, living a lifestyle that often includes interactions with individuals with infectious diseases and sex-barter for drugs. Such choices expose them to more significant risks of contracting infections from blood-borne pathogens such as HIV and Hepatitis B or C virus.
Furthermore, the use of intravenous drugs, contaminated drugs, sharing needles and inadequate sterilization of drug paraphernalia puts them at high risk for localized and systematic infections such as cellulitis, abscesses, endocarditis, and osteomyelitis.
Higher rates of depression, risky sexual behaviors and other psychosocial disorders that result in incarceration and failed relationships are common among OUD patients. The suicidal risk is significantly higher in this population as well. As a result, OUD patients who do not die from overdose often die prematurely of other such causes.
In a U.S. national cohort study of OUD in the first year after nonfatal opioid overdose, there was a marked excess of deaths attributable to a wide range of substance use associated mental health and medical conditions. The most common causes of death were substance use-associated diseases (26.2 percent), diseases of the circulatory system (13.2 percent), and cancer (10.3 percent).
Specific causes included HIV, chronic respiratory diseases, viral hepatitis, and suicide. This data only reiterates the dire need to secure the fate of untreated OUD and hence, the urgent need for better treatments.
Drop-outs
Here, it is also important to mention the patients who drop-out mid-treatment without fully recovering.
Just like in patients with a concussion or Traumatic Brain Injury, patients typically report a loss of function and are reluctant to get themselves evaluated or treated. Such patients typically almost always relapse immediately and may be victims of an overdose.
It is crucial to test treatments not just for safety, but for efficacy as well, that focus on long-term recovery. Awareness about the repercussions of substance abuse on the brain and associated health concerns need to be discussed in detail with the patients to make them realize just how crucial it is to get the necessary treatment.
Looking forward
PHP care management had put together a program four decades ago to improve all treatment outcomes. It is real, possible and understandable. The key to its success is the commitment to living drug-free, the active and sustained testing for any use of alcohol or other drugs linked to prompt intervention to any relapse, the use of recovery support, and the long duration of active care management: 5 years.

This approach is rarely seen in the current addiction treatments, which often is siloed out of mainstream medicine – with little or no monitoring or support after the typically short duration of treatment.
Yet, an even larger lesson can be learned from the millions of Americans now in recovery from addiction to opioids and other drugs. The “evidence” of what recovery is and how it is achieved and sustained is available to everyone who knows or comes into contact with people in recovery. The millions of Americans in recovery are the inspiration for a new generation of improved addiction treatment.
Findings from recent studies, further consolidate the fact that addiction is a severe and chronic disorder that can be treated successfully over extended periods in a large percentage of people. SUDs need not be viewed as inevitably leading to relapse and lengthy addiction careers.
With an all-encompassing, evidence-based and holistic approach, addicted patients can once again regain control of their lives. On the basis of these findings, there is a reason for renewed optimism among individuals with SUDs and their families.
Please See
References
1. https://www.health.harvard.edu/blog/is-addiction-a-brain-disease-201603119260
2. https://www.ncbi.nlm.nih.gov/books/NBK458661/
3. https://csam-asam.org/sites/default/files/pdf/misc/JSAT_2009_DuPont.pdf
4. https://www.mdedge.com/psychiatry/article/176922/addiction-medicine/beyond-opioids
About the Author:
 Mark S. Gold, M.D. served as Professor, the Donald Dizney Eminent Scholar, Distinguished Professor and Chair of Psychiatry from 1990-2014. Dr. Gold was the first Faculty from the College of Medicine to be selected as a University-wide Distinguished Alumni Professor and served as the 17th University of Florida’s Distinguished Alumni Professor.
Mark S. Gold, M.D. served as Professor, the Donald Dizney Eminent Scholar, Distinguished Professor and Chair of Psychiatry from 1990-2014. Dr. Gold was the first Faculty from the College of Medicine to be selected as a University-wide Distinguished Alumni Professor and served as the 17th University of Florida’s Distinguished Alumni Professor.
Learn more about Mark S. Gold, MD
About the Transcript Editor:
 A journalist and social media savvy content writer with extensive research, print and on-air interview skills, Sana Ahmed has previously worked as staff writer for a renowned rehabilitation institute, a content writer for a marketing agency, an editor for a business magazine and been an on-air news broadcaster.
A journalist and social media savvy content writer with extensive research, print and on-air interview skills, Sana Ahmed has previously worked as staff writer for a renowned rehabilitation institute, a content writer for a marketing agency, an editor for a business magazine and been an on-air news broadcaster.
Sana graduated with a Bachelors in Economics and Management from London School of Economics and began a career of research and writing right after. Her recent work has largely been focused upon mental health and addiction recovery.
The opinions and views of our guest contributors are shared to provide a broad perspective of addictions. These are not necessarily the views of Addiction Hope, but an effort to offer a discussion of various issues by different concerned individuals.
We at Addiction Hope understand that addictions result from multiple physical, emotional, environmental and genetic factors. If you or a loved one are suffering from an addiction, please know that there is hope for you, and seek immediate professional help.
Published on October 15, 2018
Reviewed by Jacquelyn Ekern, MS, LPC on October 15, 2018
Published on AddictionHope.com
