
Contributor: Mark S. Gold, M.D., Professor, Washington University School of Medicine - Department of Psychiatry
Three Phases of Buprenorphine Treatment:
The Induction Phase is the medical initiation of buprenorphine treatment. Phase 1 usually begins with a visit to a qualified physician's office or certified OTP using approved buprenorphine products.
Buprenorphine is administered to a person with a diagnosis of an OUD and who is in the early stages of opioid withdrawal. We try to give it to people who have abstained from using opioids for 12 to 24 hours.
Buprenorphine can also cause acute withdrawal in those patients. It is not generally a problem but can be avoided by giving Buprenorphine to patients who are in the early stages of withdrawal and who do not have methadone or other opioids in their bodies. The clinician documents the objective signs of withdrawal and begins treatment with a dose of 2 to 4 mg buprenorphine. This initial dose may be increased in increments of 2 to 8 mg.
The Stabilization Phase begins after an OUD patient has successfully discontinued or significantly reduced their opioid use, no longer has opioid cravings, and is described as stable and without side effects. The buprenorphine dose may need to be individualized during this stabilization phase.
Following initiation, the buprenorphine dose is titrated to alleviate symptoms. Clinical evidence suggests that 16mg per day is more effective than lower doses. We do not generally use doses higher than 24mg per day as there is little evidence that they improve outcomes, and higher doses may increase the risk of diversion [9].
The Maintenance Phase is defined by the patient being stable, doing well on a steady dose of Buprenorphine, and is starting to be able to think about their life, goals, and engage in treatment [10]. There is no ideal length of time for the maintenance phase. Rather than an absolute time, the best guidance is to individualize treatment and consider as long as possible as the ideal.
The treatment works but must be initiated. Many patients who have been rescued from an overdose are not given a MAT [11]. It may be worthwhile to consider starting Buprenorphine and asking [12] what is the worst thing that could happen" after giving a patient Buprenorphine?
Not recognizing that: The patient has other opioids on board that will be displaced from the receptors by Buprenorphine, and you can precipitate severe withdrawal [13]. ASAM's newest guidelines recommend that Buprenorphine should not be initiated until there are objective signs of opioid withdrawal, as this method reduces the risk of precipitated withdrawal [14].
Another possibility was that the patient was experimenting with opioids and did not meet the criteria for an opioid use disorder. Physicians can receive Buprenorphine training and waiver through The American Society of Addiction Medicine, which offers this training curriculum [15]. Treatment of OUDs is most effective in combination with counseling and psychiatric services, which can include different forms of behavioral therapy, medications, and self-help programs.
OTPs
 In the United States, the treatment of opioid dependence with medications is governed by the Certification of Opioid Treatment Programs, 42 Code of Federal Regulations (CFR) 8. This regulation created a system to accredit and certify opioid treatment programs (OTPs).
In the United States, the treatment of opioid dependence with medications is governed by the Certification of Opioid Treatment Programs, 42 Code of Federal Regulations (CFR) 8. This regulation created a system to accredit and certify opioid treatment programs (OTPs).
OTPs provide medication-assisted treatment (MAT) for people diagnosed with an opioid-use disorder. MAT patients also must receive counseling, which can include different forms of behavioral therapy.
Stigma
All of the behavioral health, psychiatric, and addiction medication-assisted treatment is limited by lack of insurance parity, access, and stigma. The ability to get Buprenorphine from your physician or health professionals is by itself de-stigmatizing.
The properties of the medication also reduce diversion and concern that we are not treating the OUD but rather replacing one opioid with another. Buprenorphine is available in many formulations. But, the most common formulation prescribed of Buprenorphine and Naloxone (Suboxone) is in a 4:1 ratio of agonist: antagonist.
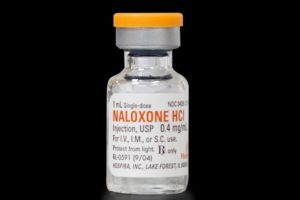
As an opioid antagonist with high first-pass hepatic metabolism, Naloxone does not affect the sublingual use of Buprenorphine but blocks intravenous or intranasal abuse of Buprenorphine. Reducing deaths, overdoses, drive for opioids, and stabilizing the OUD to the point that counseling and therapy can progress, has increased acceptance of Buprenorphine as being treatment and solution, rather than being part of the problem.
In seeking to respond to the opioid crisis and OUD, we have tried to lower barriers to treatment and use digital and telephone tele-addiction medicine. Other options, including changing the laws around methadone to expand access, have also proposed by MAT experts [16].
Diversion and Abuse of Buprenorphine
Buprenorphine and Buprenorphine+Naloxone are opioids, and diversion can and does happen. Diverted Buprenorphine has less street value, is less reinforcing than diverted full agonist opioids that cause greater euphoria, respiratory depression, and overdose.
Buprenorphine's opioid effects are still appealing to users who do not have an opioid dependency [17]. Suboxone takes Buprenorphine and adds Naloxone to decrease the likelihood of street sales and diversion, but intravenous abuse occurs.
SUD patients know that sublingual tablets can be crushed and injected. Usually, the naloxone effect dominates and can block the euphoric effect. But, the blockade is only relevant up to a point.
For abusers with OUDs, intravenous use can bring on opiate withdrawal symptoms. Still, this is not commonly the reason for buying buprenorphine or buprenorphine + naloxone on the street.
Cicero and others have shown that people buying diverted Buprenorphine are usually trying to self-medicate [18], prevent opioid withdrawal, and not generally trying to experience euphoria. According to ASAM's recent guidelines, clinicians should take steps to keep vigilant and reduce the chance of buprenorphine diversion when possible.
 Recommended strategies must be tempered by COVID 19 realities. But, generally, diversion reduction strategies suggested by ASAM are: include frequent office visits (e.g., weekly in early treatment); drug testing, including testing for Buprenorphine and metabolites; and recall visits for medication counts [19].
Recommended strategies must be tempered by COVID 19 realities. But, generally, diversion reduction strategies suggested by ASAM are: include frequent office visits (e.g., weekly in early treatment); drug testing, including testing for Buprenorphine and metabolites; and recall visits for medication counts [19].
Length of Time in Treatment and Detoxification
According to ASAM's new OUD treatment guidelines [20], treatment duration should be as long as possible or needed. Some patients may want to transition to an injectable or to injectable Naltrexone.
Buprenorphine taper and discontinuation can be perceived as too slow by some patients, but it is actually a slow process with close monitoring over months. Patients who discontinue buprenorphine treatment like those who leave the treatment program should be made aware of the increased risk of death if they return to illicit opioid use.
Patients should be encouraged to remain in treatment if possible, to prevent slips, relapses, and overdoses. It is generally a good idea to aspire to have a program-wide follow-up plan for all patients in residential or outpatient treatment for an OUD to have ongoing monitoring for a year past the point of discontinuation.
Conclusions
Addiction Medicine has made significant progress in developing evidence-based treatments for OUDs, opioid overdose, and rescues. MAT treatment works and saves lives.
Sadly, OUDs and opioid overdose and deaths of despair have increased and brought much-needed attention to the evaluation and treatment of OUDs. Treatments include EMT and community treatment for an overdose with naloxone-Narcan, and evidence-based treatment of OUD with Buprenorphine, buprenorphine-naloxone, methadone, and naltrexone [21].
MATs are now an essential part of an intensive residential or outpatient programs. They are also the central part of the treatment in methadone or OTPs. All of the MATs have a role in the treatment, and throughout a patient with an OUD's life, several different medicines may be indicated.
Our work in the laboratory [22] suggested that Buprenorphine would be an ideal MAT for fentanyl use disorders and withdrawal. Unfortunately, patients with OUD often come into treatment in an emergency. They have numerous emergency room in and out of treatment.
Doing an evaluation and treating the co-morbidity helps. That means providing medications plus medical, infectious, family, vocational, preventative, psychological, and psychiatric services. Few survivors of opioid overdose find treatment than we would like.
 This may be partially explained by well-documented challenges of oral rather than extended-release injectable MATs. While beyond the scope of this review on Buprenorphine, injectable, and long-acting Buprenorphine.
This may be partially explained by well-documented challenges of oral rather than extended-release injectable MATs. While beyond the scope of this review on Buprenorphine, injectable, and long-acting Buprenorphine.
Probuphine (Buprenorphine) implant for subdermal administration and Sublocade (buprenorphine extended‐release) injection for subcutaneous use are long-acting alternatives that can be used in stable patients. Buprenorphine is prescribed more than other MAT treatments for OUD.
But, that does not mean that only Buprenorphine or Buprenorphine + Naloxone is a logical choice for a particular patient. Patients with OUD have a chronic and relapsing life-long disease for which we do not have a cure.
But, which treatment is best for which person, is not well understood. We also do not pay much attention to treatment resistance [23] and offer the same treatment approach, many times to the same person, even though they relapsed.
Please see - Buprenorphine, Suboxone and the Treatment of Opioid Use Disorder (OUD) in 2020 - Part 1
References:
9. The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update. J Addict Med. 2020;14(2S Suppl 1):1-91. doi:10.1097/ADM.0000000000000633
10. https://www.samhsa.gov/medication-assisted-treatment/treatment/buprenorphine
11. https://medicine.yale.edu/edbup/resources/
12. https://www.drugabuse.gov/nidamed-medical-health-professionals/discipline-specific-resources/emergency-physicians-first-responders/initiating-buprenorphine-treatment-in-emergency-department/frequently-asked-questions-about-ed-initiated-buprenorphine
14. The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update. J Addict Med. 2020;14(2S Suppl 1):1-91. doi:10.1097/ADM.0000000000000633
15. https://www.asam.org/education/live-online-cme/waiver-qualifying-training
16. Bell J, Strang J. Medication Treatment of Opioid Use Disorder. Biol Psychiatry. 2020;87(1):82-88. doi:10.1016/j.biopsych.2019.06.020
17. https://www.samhsa.gov/medication-assisted-treatment/treatment/buprenorphine
18. Cicero TJ, Ellis MS, Chilcoat HD. Understanding the use of diverted Buprenorphine. Drug Alcohol Depend. 2018;193:117-123. doi:10.1016/j.drugalcdep.2018.09.007
19. https://journals.lww.com/journaladdictionmedicine/pages/articleviewer.aspx?year=2020&issue=04000&article=00004&type=Fulltext
20. The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update. J Addict Med. 2020;14(2S Suppl 1):1-91. doi:10.1097/ADM.0000000000000633
21. Oesterle TS, Thusius NJ, Rummans TA, Gold MS. Medication-Assisted Treatment for Opioid-Use Disorder. Mayo Clin Proc. 2019;94(10):2072-2086. doi:10.1016/j.mayocp.2019.03.029
22. Bruijnzeel AW, Marcinkiewcz C, Isaac S, Booth MM, Dennis DM, Gold MS. The effects of Buprenorphine on fentanyl withdrawal in rats. Psychopharmacology (Berl). 2007;191(4):931-941. doi:10.1007/s00213-006-0670-2
23. Patterson Silver Wolf DA, Gold M. Treatment resistant opioid use disorder (TROUD): Definition, rationale, and recommendations. J Neurol Sci. 2020;411:116718. doi:10.1016/j.jns.2020.116718
About the Author:
 Mark S. Gold, M.D., Professor, Washington University School of Medicine - Department of Psychiatry, served as Professor, the Donald Dizney Eminent Scholar, Distinguished Professor and Chair of Psychiatry from 1990-2014.
Mark S. Gold, M.D., Professor, Washington University School of Medicine - Department of Psychiatry, served as Professor, the Donald Dizney Eminent Scholar, Distinguished Professor and Chair of Psychiatry from 1990-2014.
Dr. Gold was the first Faculty from the College of Medicine to be selected as a University-wide Distinguished Alumni Professor and served as the 17th University of Florida’s Distinguished Alumni Professor.
Learn more about Mark S. Gold, MD
The opinions and views of our guest contributors are shared to provide a broad perspective of addictions. These are not necessarily the views of Addiction Hope, but an effort to offer a discussion of various issues by different concerned individuals.
We at Addiction Hope understand that addictions result from multiple physical, emotional, environmental and genetic factors. If you or a loved one are suffering from an addiction, please know that there is hope for you, and seek immediate professional help.
Published on July 24, 2020
Reviewed by Jacquelyn Ekern, MS, LPC on July 24, 2020
Published on AddictionHope.com
