
Opioids are a class of drugs that include illegal drugs like heroin as well as prescription drugs like fentanyl, oxycodone (OxyContin®), hydrocodone (Vicodin®), codeine, morphine, and many others. [5]
While not everyone who is prescribed or has tried opioids will go on to abuse them, they are highly addictive due to their powerful ability to reduce physical pain and induce feelings of euphoria. [5]
Opioid abuse has continued to increase over the past several years, and the crisis is expected to worsen in the next decade. Every day, more than 130 people in the United States die after overdosing on opioids.[1, 2, 3, 4, 5]
 A recent study states that, unlike historical trends where prescription opioid use has served as a path to heroin use, more people are directly initiating opioid use with illicit opioids.
A recent study states that, unlike historical trends where prescription opioid use has served as a path to heroin use, more people are directly initiating opioid use with illicit opioids.
Moreover, other studies have illuminated that the rapid increase in illicit opioid lethality is likely primarily driven by the infiltration of the heroin supply with the highly potent synthetic opioid called fentanyl. [6, 7, 8]
Opioid abuse and overdose is a severe national crisis that affects public health as well as social and economic welfare. The Centers for Disease Control and Prevention estimates that the total "economic burden" of prescription opioid misuse alone in the United States is $78.5 billion a year, including the costs of healthcare, lost productivity, addiction treatment, and criminal justice involvement. [4]
Unfortunately, the opioid crisis is only expected to worsen. By 2025, the annual number of opioid overdose deaths is projected to reach nearly 82,000, resulting in approximately 700,000 deaths from 2016 to 2025. [2]
According to a recent publication in The Journal of American Medical Association Network, the most effective interventions to prevent opioid abuse and overdose are likely to include: [2]
- Screening for opioid abuse in all relevant health care settings
- Improving access to medications for opioid abuse such as methadone and buprenorphine
- Increasing opioid abuse training programs at medical and nursing schools
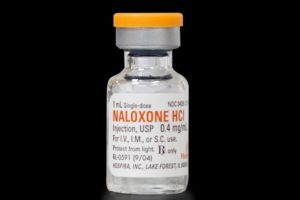
- Improving access to harm-reduction services such as overdose-reversing drugs
- Improving access to opioid abuse treatment
- Controlling the supply of illicit opioids
- Lowering exposure to illicit opioids
- Reducing the stigma of opioid use and abuse
 In response to the opioid crisis, the U.S. Department of Health and Human Services is focusing its efforts on five major priorities: [4]
In response to the opioid crisis, the U.S. Department of Health and Human Services is focusing its efforts on five major priorities: [4]
- Improving access to treatment and recovery services
- Promoting the use of overdose-reversing drugs
- Strengthening the understanding of the epidemic through better public health surveillance
- Providing support for cutting-edge research on pain and addiction
- Advancing better practices for pain management
Sources:
1. Substance Abuse Center for Behavioral Health Statistics and Quality. (2017, Sept 7). Results from the 2016 National Survey on Drug Use and Health: Detailed Tables. SAMHSA. Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.htm. on 2019, Feb 19.
2. Chen Q, Larochelle MR, Weaver DT, et al. (2019). Prevention of Prescription Opioid Misuse and Projected Overdose Deaths in the United States. JAMA Netw Open, 2(2):e187621. doi:10.1001/jamanetworkopen.2018.7621
3. Rudd, R.A., Seth, P., David, F., Scholl, L. (2016). Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Report; 65 (50-51) : 1445-1452. doi:10.15585/mmwr.mm655051e1.
4. National Institute on Drug Abuse. (2010, Feb 19). Opioid Overdose Crisis. Retrieved fromhttps://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis on 2019, Feb 19.
5. NIDA. Opioids. Retrieved from https://www.drugabuse.gov/drugs-abuse/opioids on 2019, Feb 19.
6. Cicero TJ, Ellis MS, Kasper ZA. Increased use of heroin as an initiating opioid of abuse. Addict Behav. 2017;74:63-66. doi:10.1016/j.addbeh.2017.05.030
7. Frank RG, Pollack HA. Addressing the fentanyl threat to public health. N Engl J Med. 2017;376(7):605-607. doi:10.1056/NEJMp1615145
8. O’Donnell JK, Halpin J, Mattson CL, Goldberger BA, Gladden RM. Deaths involving fentanyl, fentanyl analogs, and U-47700—10 states, July-December 2016. MMWR Morb Mortal Wkly Rep. 2017;66(43):1197-1202. doi:10.15585/mmwr.mm6643e1
About the Author:
 Chelsea Fielder-Jenks is a Licensed Professional Counselor in private practice in Austin, Texas. Chelsea works with individuals, families, and groups primarily from a Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) framework.
Chelsea Fielder-Jenks is a Licensed Professional Counselor in private practice in Austin, Texas. Chelsea works with individuals, families, and groups primarily from a Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) framework.
She has extensive experience working with adolescents, families, and adults who struggle with eating, substance use, and various co-occurring mental health disorders. You can learn more about Chelsea and her private practice at ThriveCounselingAustin.com.
The opinions and views of our guest contributors are shared to provide a broad perspective of addictions. These are not necessarily the views of Addiction Hope, but an effort to offer a discussion of various issues by different concerned individuals.
We at Addiction Hope understand that addictions result from multiple physical, emotional, environmental and genetic factors. If you or a loved one are suffering from an addiction, please know that there is hope for you, and seek immediate professional help.
Published on March 4, 2019
Reviewed by Jacquelyn Ekern, MS, LPC on March 4, 2019
Published on AddictionHope.com
